Does this doctor hold the secret to ending malaria?
From his extensive laboratory on the leafy campuses of the University of Oxford, Professor Adrian Hill is conjuring up a formula to protect us from disease.
As director of the Jenner institute, Hill is creating a well-crafted "potion" of ingredients which, when combined inside a vaccine, could prepare our immune system to attack biological invaders.
His formulation could one day form the foundation to protect humans from a range of diseases including malaria, HIV and tuberculosis. He is designing a new class of vaccine, unlike any other in use today, with an end goal of disease elimination.
"This is being assessed widely for use in cancer, Hepatitis C, and we've used it in Ebola and HIV," says Hill. "There are 8 different diseases where [this] approach is in clinical trial."
Not all of these trials are being led by Hill, but he has pioneered the protocol for testing these vaccines in humans -- not just mice or monkeys like many before him. He trialled Ebola vaccines during the 2014 epidemic and his institute has one in development for Zika.
However, his desire to create vaccines began with a wish to stop one particular disease -- malaria.
As a young medical student, aged 20, Hill had visited his uncle in what was then Rhodesia (now Zimbabwe) and was shocked by the health issues there.
"Not only was there a huge amount of disease and very little medical care, but also a war," says Hill. As he traveled around the African continent for research in subsequent years, he saw the true extent of the malaria epidemic.
"I was really overwhelmed by the scale of the problem," says Hill. "It became clear to me that what the world needed was a vaccine against malaria."
The need for a vaccine
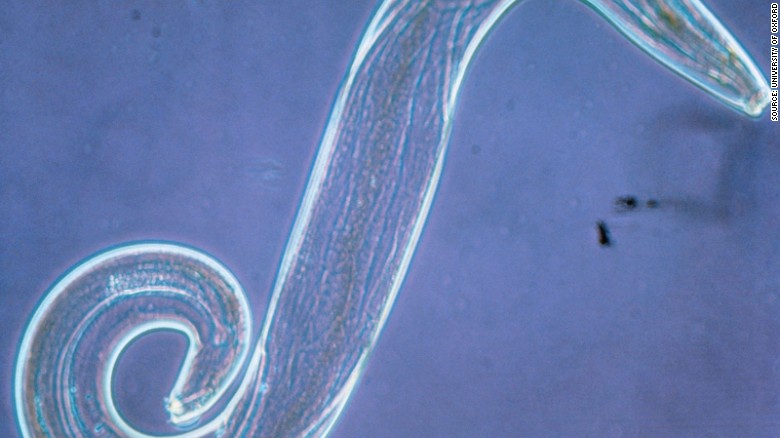
Hill's desire to eliminate malaria is an ambitious goal. The parasite behind the disease -- Plasmodium falciparum -- infected 214 million people in 2015, and caused more than 430,000 deaths.
"[If we] compare this with Ebola ... the same year we had almost 500,000 malaria deaths ... if malaria was new and suddenly killing half a million people on the continent and hadn't been doing that before there would be a global panic," says Hill.
If malaria was new and suddenly killing half a million people on the continent...there would be a global panic
Prof. Adrian Hill, University of Oxford
The numbers affected have fallen over the last decade, coming down from more than 1 million deaths each year, thanks mostly to the effective use of insecticide-treated bed nets, insecticide spraying in homes, and the development of combination drug therapies. But resistance has now emerged, most notably in South-East Asia, against both the drugs and insecticides, and is likely to spread.
A more sustainable solution is needed -- such as a vaccine -- and Hill is determined to make it happen.
During more than 20 years working on vaccines, he has tested tens of vaccines in humans, 55 of them just on malaria, to eventually find out they are not effective.
While for some this would be demoralizing, for Hill each is just another hurdle on the way to the finish line.
How his vaccine would work
The immune response of a human is an extremely complex beast that experts are still yet to fully understand. Vaccines, however, generally work by making the body believe it is infected and gearing up the adaptive immune system to fight this supposed infection using antibodies -- having them primed and ready for future infections.
Current vaccines, such as those used against measles, tetanus or polio, work in this way, generating antibodies that flag future infections for other immune cells to attack. But this effect isn't quite enough to fight more complicated diseases, such as malaria.
The plasmodium parasite has many routes of attack, a complicated life cycle with multiple stages of development, and thousands more genes than other disease-causing bugs.
"With malaria you've got 5,000 genes, so you've got to figure out the best [ones] to put in the vaccine," says Hill. The genes create proteins once inside the body to kick start immunity against the parasite.
"If you just look historically when people have tried to protect against malaria with just antibodies, it has not worked," says Helen Fletcher, a former colleague of Hill at Oxford who is now senior lecturer in Immunology at the London School of Hygiene and Tropical Medicine.
So Hill is going for a whole new approach.
"Our vaccine works in a fundamentally different way," he says. "We're targeting the cellular arm of the immune system."
This "arm" is the home of a different group of cells, known as T-cells. His team are specifically targeting CD8 T-cells, known as killer cells, which have the ability to kill any cells that are infected, as well as cancer cells. The challenge is getting enough of them.
"The problem is we need probably of the order of 2,000 to get good efficacy," he says. That led to the development of his latest formula -- a combination of two viruses that have been given the DNA of the malaria parasite. The virus-containing vaccines are injected into people on two separate occasions, to first prime the body, then boost the immune response.
The strategy is aptly called the prime-boost approach.
How to prime
After years of trialling different combinations of viruses, Hill's team believe they have a winning formula.
"I remember where I was standing when I first saw the result of prime-boost, not in humans but in mice; suddenly from getting no protection we were getting every mouse protected," says Hill.
They had seen 100% protection against malaria in mice, after previous attempts showing just 20%.
"That was a very memorable moment, in 1996, as then I knew we were onto something," he says.
They soon decided on a particular pairing of viruses which each have DNA from the malaria parasite inserted. Immunization begins with an injection of a modified adenovirus that typically infects chimps (CHA) and a later injection of a modified Vaccinia Ankara (MVA) virus acting as a booster.
"That is a non-obvious thing to do -- nearly every vaccine you get is given as the same composition once, twice or three times," says Hill.
They were soon seeing thousands of T-cells being generated, primed to attack infected cells.
From mice to people
Hill's vaccine was recently trialled in humans, among 121 adults in Kenya, andwas 67% effective in preventing malaria for eight weeks following the injection.
"That is probably one of the best results ever in the malaria vaccine field," says Hill.
But his target age group is infants.
"We always wanted to vaccinate the younger infants because you don't get malaria until you're about 6 months of age, so [we want to get] the vaccines in before that," says Hill.
Field trials in infants are at least one year away, but Hill is determined to make it happen.
"I think the prime boost approach is the best strategy that we have [against] these difficult pathogens," says Fletcher, whose own research focuses on vaccines for tuberculosis.
Hill hopes his current vaccine will enter the final stage clinical trials by 2022, in order to have a vaccine licensed for use by 2025.
But he has even greater ambitions for his future vaccines.
Four in one
While Hill's current vaccine design targets malaria at one of its earliest stages, when it enters the liver, this is just one of multiple stages through which the malaria parasite causes its damage. Four of these stages are prime targets for an immune attack and Hill wants to take on each of them -- using one extra potent vaccine.
"If you got partially effective vaccines with efficacy that's 30 % maybe 60% on an ideal setting, why wouldn't you use all the components to maximize efficacy?" says Hill.
His team at the Jenner Institute have a range of vaccines in development that target each of these four stages. If results are good in future trials, they hope to one day combine them all together.
The most success in developing a vaccine against malaria has, to date, been by pharmaceutical giant GSK. In 2015, their RTS,S vaccine, trade name Mosquirix, was shown to partially protect infants and young children from developing malaria. But it wasn't quite enough for the World Health Organization (WHO) to recommend its use in infants, and in January 2016 the organization called for pilot programs to test its effectiveness among young children in a real-world setting. While this happens, Hill is hoping to improve his vaccine and trial it in infants so it is ultimately a more effective option.
"Malaria is [his] original passion and original research interest, but what a target...it's such a difficult pathogen to work with," says Fletcher. "But maybe that's what keeps him interested."
Could Hill hold the future solution to truly ending malaria?
"We'll let you know in 2025," he says. "It's looking as if it may be doable, [so] we think this is going to work."
News Courtesy: www.cnn.com